Digestive Health Specialists on Supporting Your Microbiome
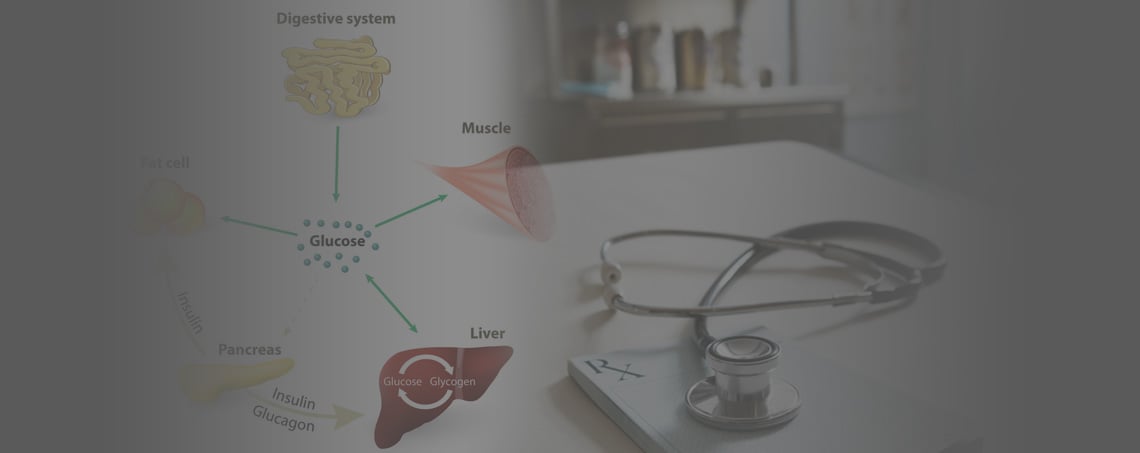
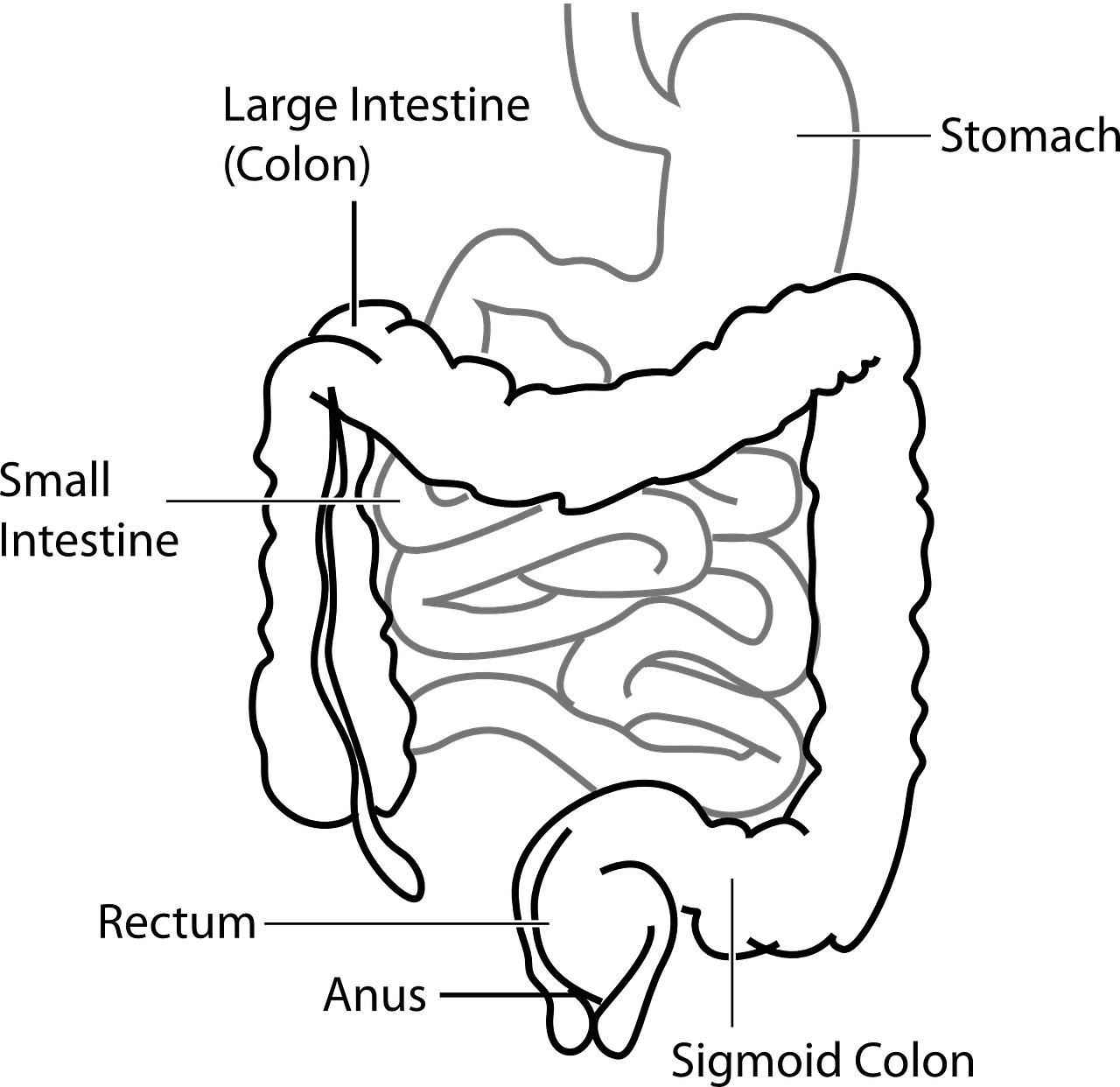
Your digestive health is determined by how effective your digestive tract is at breaking down down and absorbing the food you consume. The system itself appears quite simple on the surface consisting of the gastrointestinal tract, which extends from the mouth to the anus, and other accessory organs such as the liver, pancreas, and gall bladder. However, as digestive health specialists point out, this tubular organ is very complex relying on many feedback loops and performing many functions locally and throughout the body.
The main function of your digestive tract is to process the food you eat into smaller and simpler molecules, absorb the nutrients and water, and discard the rest into feces. It is vulnerable to insults and problems at multiple points along the tract. One area that is particularly vulnerable are the many microorganisms that are naturally occurring in the digestive tract. This mass of microbes known as the microbiome determines much of your digestive health and overall health. Until recently the microbiome has not been studied much and so remained poorly understood. In this article we will explore the importance of the microbiome and how to maintain and improve the health of yours.1
Your Microbiome
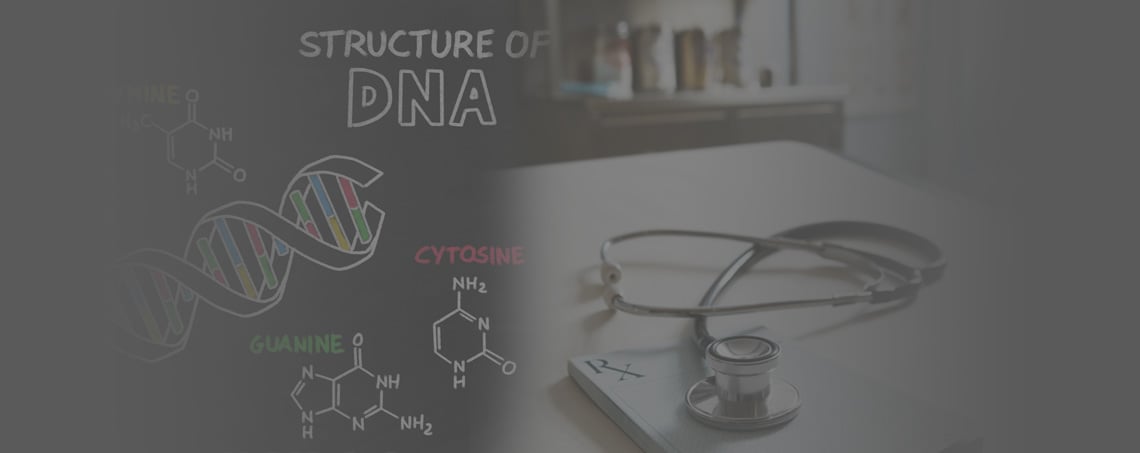
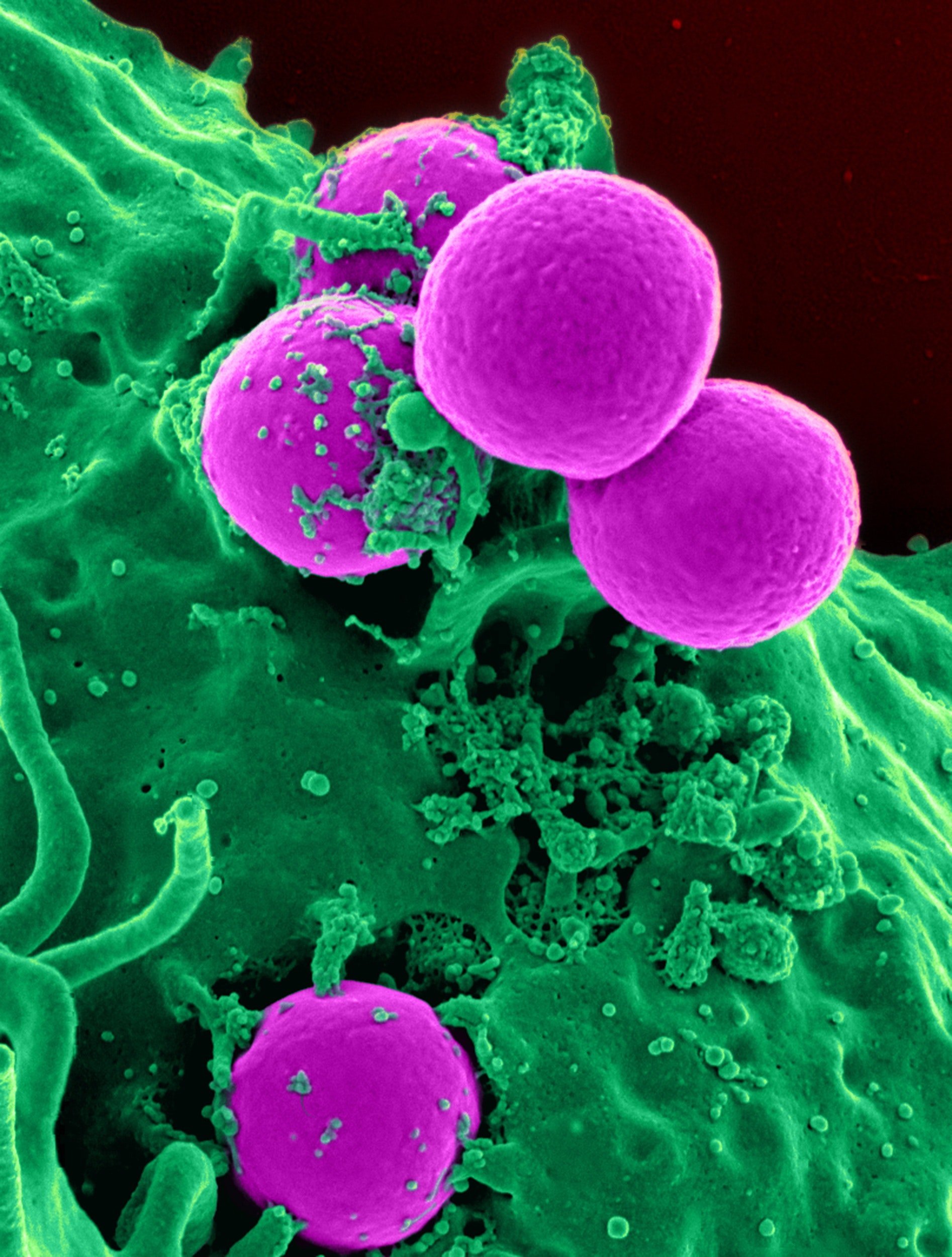
Your mirobiome is the collection of microbes (billions of them) that live on your skin and more on topic, in our digestive tract. The bulk of these microbes inhabit the large intestine while the other areas of the digestive tract contain very few. While they are very small in size, they are abundant in numbers. On average there are more bacteria in the colon than there are cells in the body and the microbial genetic material is 150 times greater than the human genetic material in our body.
With such massive numbers, it is no surprise that they play key roles in our health and digestion. While this is more obvious now than ever before our understanding of the microbiome is still in it's infancy and not fully understood. For instance, we know they aid in providing nutrition to the cells of the digestive tract and also provide vitamins to the body. We also know that microbial byproducts and metabolites are absorbed into the body and enter the blood stream. These microbial biochemicals then intermingle with the biochemicals from our body. Some of these biochemicals are good, some are toxic and most we just don't know enough about yet. The last category is important because it may hold key answers to many chronic health issues. Understanding these chemicals may take time since it requires a better understanding of the microbes themselves, their interrelationships, and what a "normal" balanced microbiome looks like.
While a more complete understanding of the microbiome is coming to light, most digestive health specialists agree that balance, diversity, and abundance are important. To illustrate this, it helps to look at the microbiome in people with unhealthy digestion.
Microbiome and Digestive Health Problems
The health of your microbiome is the common denominator behind digestive problems like Crohn's Disease, IBS (Irritable Bowel Syndrome), and SIBO (Small Intestinal Bacterial Overgrowth). Each one of these show (or represent) a disruption in the microbiome. For instance, Crohn's Disease is a chronic inflammatory condition of the digestive tract involving the entire thickness of the digestive wall (transmural granulomatous inflammation).2. The particular cause of Crohn’s disease is not known but it is conventionally thought of as an autoimmune condition having nothing to do with the microbiome. Still evidence suggests there are many risk factors outside of autoimmune ranging from genetic to environmental and even a dysregulation of the immune system. In particular the response of the immune system to microorganisms in the digestive tract. This is where balance comes in.
Alterations in the good bacteria present in the digestive tract cause them to attach to the mucus membranes in the digestive tract triggering damage, inflammation, and an immune reaction. These are all hallmarks of Cohn's disease and why many think an imbalanced microbiome is implicated. In fact many have proposed that this inflammation is caused by SIBO. SIBO itself is an excess of bacteria in the small intestines that can lead to local and systemic inflammation. SIBO patients often present with chronic diarrhea (except in SIBO constipation), abdominal pain and weight loss. These same symptoms are found in Crohn's disease patients but with Crohn's they are more severe and also have mucus and blood in stool as well. Some patients with Crohn's and SIBO can also have manifestations outside the digestive tract such as joint pain, skin rashes, etc. With so many similarities, are SIBO and Crohn's the same thing or is Crohn's a progression of SIBO?
They may be the same but some questions are still not answered. For instance, how these bacteria get in the small intestine and what causes them to cling to the intestines is still currently unknown. 2
IBS is another chronic digestive condition that affects the digestive tract and also does not have an exact known cause(s).4 Patients with IBS typically have recurrent diarrhea, or constipation or diarrhea alternating with constipation. Other digestive symptoms are common too. The main difference between Crohn’s disease and IBS is that there are no structural or deep cellular changes such as inflammation and ulcerations in IBS. It is therefore regarded as a functional disorder.4 Nevertheless, alteration in the content of microorganisms within the digestive tract are also strongly implicated.
Because of the alteration in the microbiome of those with IBS and Crohn's many digestive health specialists are looking at SIBO as an underlying cause for both. Indeed SIBO is found in about 30-85% of those with IBS and in about 25% of those with Crohn’s disease.5 While not everyone with IBS or Crohns has SIBO, those that don't likely do have some kind of microbiome imbalance, like dysbiosis. To understand the kinds of imbalance and what to do about it, we can explore what research shows about using probiotics for these conditions.
Role of Probiotics in Crohn’s Disease and IBS
Research shows that probiotics do help restore digestive health but the amount of help is dependent on the type of probiotic organism used and the type of digestive problem present. Regardless of the disease type probiotics have many modes of action and include:
- Maintenance of the quality of the normal microbial environment
- Eliminating the disease-causing organisms in the digestive tract
- Secretion of mucus
- Activation of the immune system to adapt to these microorganisms’ environment and to stop seeing it as foreign
- Restoring intestinal epithelial barrier (i.e. prevents the disease-causing organisms from attaching to and crossing the lining of the intestine into the body circulation)1
The use of probiotics in the treatment of Crohn's and IBS is still an area of controversy among digestive health specialists. Much of the research studies are not uniform in terms of dosage of the probiotic, the duration of treatment, the type of probiotic used, and the disease severity. All these led to different outcomes.6 Still, Moayyedi et al., in a review of many studies concluded that probiotics are efficacious in the treatment of IBS but the best probiotic organism and the size of the benefit was not clear to them. 7
In another review of 24 clinical studies, Didari et al., also concluded that probiotic is beneficial in IBS as it reduces pain and other symptoms.8 While many studies have demonstrated that probiotics are beneficial many have shown a no-benefit in the treatment of Crohn’s disease.9 This may be because the disease process is further progressed in Crohn's and requires a longer duration or more aggressive form of treatment before benefit would be seen.
Support and Maintaining Microbiome
Maintain
Our digestive tracts are inoculated with good bacteria from our mother and our environmental surroundings in childhood and as we age. Once we reach the age of around two to five years old our microbiome is very close to that of an adult. Initially the microbes present have a broad diversity. However this delicate diversity can deteriorate with age and exposure to many things that have a negative impact on the microbiome. These can include things in our food like pesticides, insecticides, artificial sweeteners, and other artificial flavoring. The food you eat on a daily basis also has an impact on the health of your microbes. For instance, if you don't consume enough fiber the bacteria don't have enough food and their numbers will be diminished over time. Some medication can also disrupt the balance of the microbes too.
Medications
Obviously medication like antibiotics and antifungals can and do kill the microbes and/or disrupt the natural balance. There are many other medications that can upset the balance as well. PPI's or proton pump inhibitors are used for acid reflux but in decreasing the stomach acid they also decrease the breakdown of our food leaving more for microbes to consume. This allows some of the microbes to expand and crowd out others. Opiate pain medications can also affect your microbiome by causing constipation, leaving more time for the microbes to consume food as it passes through the digestive tract. By avoiding these disruptors you can preserve your microbiome but what can you to improve it?
Probiotics to Improve Your Microbiome
Many different microorganisms are being used in probiotic formulas. The two genus most consistently used are lactobacillus and bifidobacterium. Various species within these two genus have varying degrees of benefit for digestive issues and there are other beneficial genus as well. Here is a link to useful PDF identifying specific probiotics for specific purposes.
Digestive health experts can help you get your restore balance to you microbiome by taking all aspects of your health into account. Testing your microbiome for quantities of microbes and any pathogenic microbes is a good place to start. They can also help you understand how your digestive symptoms relate to your other health problems. To get input from on your digestive problems click on the link below.
Reference list:
1. Gareau MG, Sherman PM, Walker WA. Probiotics and the gut microbiota in intestinal health and disease. Nature reviews Gastroenterology & hepatology. 2010;7(9):503-514. doi:10.1038/nrgastro.2010.117.
3. Ha F, Khalil H. Crohn’s disease: a clinical update. Therapeutic Advances in Gastroenterology. 2015;8(6):352-359. doi:10.1177/1756283X15592585.
4. Saha L. Irritable bowel syndrome: Pathogenesis, diagnosis, treatment, and evidence-based medicine. World Journal of Gastroenterology : WJG. 2014;20(22):6759-6773. doi:10.3748/wjg.v20.i22.6759.
5. Bures J, Cyrany J, Kohoutova D, et al. Small intestinal bacterial overgrowth syndrome. World Journal of Gastroenterology : WJG. 2010;16(24):2978-2990. doi:10.3748/wjg.v16.i24.2978
6. Hosseini A, Nikfar S, Abdollahi M. Are probiotics effective in management of irritable bowel syndrome? Archives of Medical Science : AMS. 2012;8(3):403-405. doi:10.5114/aoms.2012.29396.
7. Moayyedi P, Ford A, Talley N et al. The efficacy of probiotics in the treatment of irritable bowel syndrome: a systematic review. Gut. 2008;59(3):325-332. doi:10.1136/gut.2008.167270.
8. Didari T, Mozaffari S, Nikfar S, Abdollahi M. Effectiveness of probiotics in irritable bowel syndrome: Updated systematic review with meta-analysis. World Journal of Gastroenterology : WJG. 2015;21(10):3072-3084. doi:10.3748/wjg.v21.i10.3072.
9. Verna EC, Lucak S. Use of probiotics in gastrointestinal disorders: what to recommend? Therapeutic Advances in Gastroenterology. 2010;3(5):307-319. doi:10.1177/1756283X10373814.